4 Questions On NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
4 min read
![]() Dr. Andrea Gruszecki, ND
:
March 14, 2023 at 8:30 AM
Dr. Andrea Gruszecki, ND
:
March 14, 2023 at 8:30 AM

March 17th is fast approaching, and those of us that celebrate a gluten-free St. Patrick’s day have some decisions to make. The luck of the Irish may not be enough to keep our patients safe. Aside from the 20 ppm gluten-free standard, there are no FDA-mandated tests for gliadin, prolamins or allergenic grain proteins in alcoholic beverages, and no universal standards to estimate risk, should such testing be required. For now, it is an individual choice to imbibe spirits or beers that may contain potentially harmful gluten, gliadin, molecular mimics or allergens. Fortunately, US BioTek offers Celiac, IgE allergy and IgG, IgA sensitivity testing to evaluate such patients and better estimate risks.
Because the 3-day feast of St. Patrick provided a welcome relief from Lenten fasting and alcohol abstinence in the past, the holiday is now often associated with alcohol and special foods. While some of us may choose to bake our own gluten- or wheat-free porter cakes, scones or soda breads, very few of us are likely to brew our own gluten-free or wheat-free beers (green or otherwise). For those that might prefer a drop of Uisce beatha (whiskey), how do we know what is safe to drink? Our patients will turn to us for the answer.
In order to answer properly, clinicians need to understand the different proteins in wheat and gluten grains, and the types of reactions that can occur with exposure to those proteins. There is a difference in exposure risks between those with Celiac disease, IgG/IgG4 non-Celiac gluten sensitivity (NCGS) and those with IgE wheat allergy.
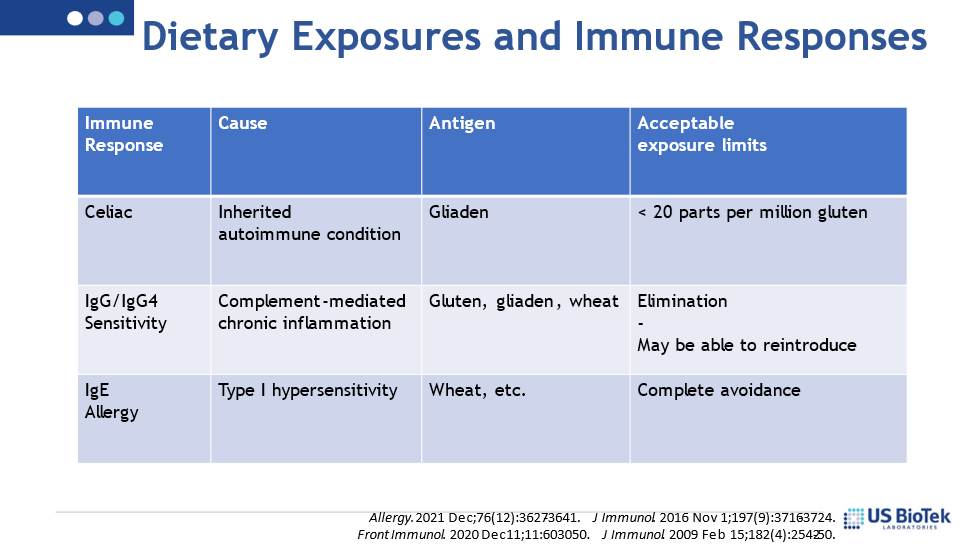
In order to manifest Celiac disease, an individual must be genetically predisposed to Celiac disease, via both HLA-DQ2/DQ8 and non-HLA genes, which results in an autoimmune disorder that damages the small intestine when there is gluten exposure. Gluten is composed of two different proteins – gliaden and glutenin. Gliadin is released from gluten during the digestive process. The gliadin then binds to specific receptors in the gut lining and induces an inflammatory response that destroys the gut lining and prevents proper digestion and assimilation. The risk of Celiac disease activation is increased when there are gut microbiome disruptions, other digestive disorders or viral pathogen exposures.
IgG/IgG4 food sensitivity may also be induced when there are microbiome disruptions or other inflammatory events that confuse the immune system and result in a loss of tolerance. Large, frequent doses of similar foods (wheat, wheat products, gluten) are common in Western diets and can induce non-allergy, non-Celiac immune responses. These immune responses typically involve antibodies such as IgG1-3 and IgG4. High levels of IgG1-3 are pro-inflammatory and may result in local or systemic symptoms hours to days after exposure. Non-Celiac gluten sensitivity (NCGS) is associated with IgG/IgG4 antibodies. NCGS patients often have higher anti-gliadin IgG4 antibodies and eosinophil counts than Celiac patients do. While NCGS causes a variety of systemic symptoms, it does not cause the same type of gut wall destruction that Celiac disease does.
Finally, an individual can be IgE-allergic to wheat, gluten, gliadin or other grains and have a classic type I hypersensitivity reaction to ingestion. Allergic responses to foods can be systemic, but often affect the digestive tract and can result in inflammation, diarrhea or constipation, in addition to more classic IgE allergy symptoms (itchy ears, lips or tongue, wheezing, throat swelling, etc.). Ideally, patients with true allergy completely avoid the allergen.
Now that we have a better understanding of the immune responses – back to the booze!
Spirits (distilled “hard alcohol”) are generally below 20 of gluten, but studies have not been done to determine the presence of other grain-based proteins such as gliadin or molecular mimics called prolamins. Prolamins have been shown to induce gluten-like small intestine damage in Celiac small intestine samples.
Commercially available beers are typically brewed from wheat and/or barley. Even though there are very low levels of protein (< 3.0 grams/L), the proteins that remain after fermentation are likely to harm those with Celiac disease. It is also possible that other grain proteins could provoke an IgE-allergy response in those allergic to gluten grains, gluten, prolamins or gliadin. Commercial beers should be avoided by these patients, including beers crafted and marketed as “gluten-removed”.
But, what about gluten-free specialty beers? Even beers tested and labeled as “gluten-free” may be able to induce an IgE-allergic reaction, because some of these beers are brewed from barley or ancient wheat varieties. In addition, a recent study has demonstrated that even beer brewed from non-gluten grains may still contain prolamins, the molecular mimics that may induce symptoms in Celiac patients.
The luck of the Irish may not be enough to keep our patients safe, nor should it be relied upon. Fortunately, US BioTek offers Celiac, IgE allergy and IgG, IgA sensitivity testing to evaluate patients and better estimate the health risks of gluten, gliadin, and grain exposure.
Resources:
Alcohol and Tobacco Tax and Trade Bureau (2023) Distilled Spirits Labeling. https://www.ttb.gov/distilled-spirits/labeling Accessed 09 March 2023.
Gnodi E, Meneveri R, Barisani D. Celiac disease: From genetics to epigenetics. World J Gastroenterol. 2022 Jan 28;28(4):449-463.
Hischenhuber C, Crevel R, Jarry B, Mäki M, Moneret-Vautrin DA, Romano A, et al. Review article: safe amounts of gluten for patients with wheat allergy or coeliac disease. Aliment Pharmacol Ther. 2006 Mar 1;23(5):559-75.
Mamone G, Picariello G, Addeo F, Ferranti P. Proteomic analysis in allergy and intolerance to wheat products. Expert Rev Proteomics. 2011 Feb;8(1):95-115.
National Archives Federal Register (2020) Food Labeling; Gluten-Free Labeling of Fermented or Hydrolyzed Foods. https://www.federalregister.gov/documents/2020/08/13/2020-17088/food-labeling-gluten-free-labeling-of-fermented-or-hydrolyzed-foods Accessed 09 March 2023.
National Celiac Association (2020) Frequently Asked Questions about Alcohol on the Gluten-Free Diet. https://nationalceliac.org/frequently-asked-questions-about-alcohol-on-the-gluten-free-diet/ Accessed 09 March 2023.
Ortiz-Sánchez JP, Cabrera-Chávez F, de la Barca AM. Maize prolamins could induce a gluten-like cellular immune response in some celiac disease patients. Nutrients. 2013 Oct 21;5(10):4174-83.
Spada V, Di Stasio L, Picascia S, Messina B, Gianfrani C, Mamone G, Picariello G. Immunogenic Potential of Beer Types Brewed With Hordeum and Triticum spp. Malt Disclosed by Proteomics. Front Nutr. 2020 Jul 9;7:98.
Thompson T. Wheat starch, gliadin, and the gluten-free diet. J Am Diet Assoc. 2001 Dec;101(12):1456-9.

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...