4 Questions On NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
5 min read
![]() Dr. Andrea Gruszecki, ND
:
May 5, 2020 at 2:35 PM
Dr. Andrea Gruszecki, ND
:
May 5, 2020 at 2:35 PM

As the COVID-19 Coronavirus continues to spread, the CDC has identified certain groups that are at a higher risk for severe illness. Patients with moderate to severe asthma are one of the high-risk groups, and these individuals are encouraged to take extra precautions as the COVID-19 pandemic continues. While infection avoidance is the most important step to reduce risk, as healthcare providers we should remember that patients with moderate to severe asthma are at an increased risk of severe respiratory infection with any viral exposure, not just COVID-19. With a better understanding of how this happens, we can take positive action steps to protect our patients now and in the future.
While the most common viral respiratory infection is Rhinovirus (the common cold), there are other viral infections that can cause similar symptoms, including Coronavirus, respiratory syncytial virus [RSV], parainfluenza virus, coxsackie virus, echoviruses, adenovirus, and other picornaviruses. Exposure to these respiratory pathogens may contribute to 50% of severe asthma exacerbation in adults, and up to 80% of asthma exacerbations in children.
This occurs in asthmatics (and those with allergic atopic disease) because chronic inflammation disrupts the lung epithelial layer, which is similar in many respects to the gastrointestinal epithelium (gut lining) that we are used to thinking about and working with. The lung lining, like the gut, has its own unique microbiome, makes mucus, and protects against pathogens. A disrupted lung lining allows viruses, other pathogens, pollutants, and antigens to penetrate deeper into the lung tissue. In the deeper tissue layers there is greater antigen uptake by dendritic cells and antigen-presenting cells, which promotes more local inflammation. As the local inflammation increases it further disrupts the lung epithelial barrier and increases the risk of infections.
Viral infections are known to further increase the reactivity of the lower airways and the amount of bronchoconstriction patients experience in response to inhaled antigens or other reactive compounds. If there is prior chronic inflammation to the respiratory epithelium lining the lungs by allergens, cigarettes or air pollutants, then the reaction to a viral exposure may be more severe and cause an acute exacerbation of the patient’s asthma. In addition, higher levels of air pollution may increase the risk of severe disease from a viral pathogen. During January and February 2020, the COVID-19 death rate in Italy approached 30.5% for elderly patients. Recent evidence indicates that the highest average death rates were found in highly polluted Northern Italian areas (12%), when compared to the rest of the country (4.5%).
So, what can we do to support our asthmatic patients during the current pandemic? We might consider a modification of the 4-R’s program used for gastrointestinal repair. For lung health, our 4 R’s are Remove, Replace, Repair, and Respire.
We can identify and remove environmental triggers that increase inflammation. For asthmatics, these include both airborne and food allergy/sensitivities. Airborne inhalant antigens include insects (dust mites, cockroaches, etc.), pet dander, and pollens. Air pollution particles or aerosolized chemicals can also result in inflammation and worsen asthma. A thorough review of the patient’s home and work environment can uncover pollutant and toxic exposures, while inhalant allergy and food allergy and sensitivity testing is required to uncover hidden triggers of inflammation. Once identified, problem foods can be eliminated or rotated to minimize inflammation.
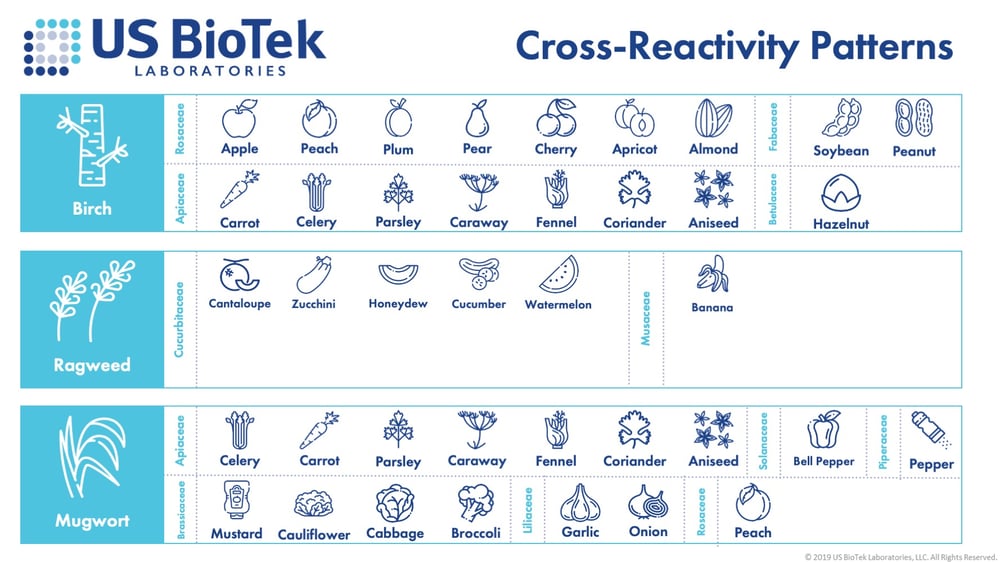
It is important to test for both inhalants and foods in asthmatic or atopic (eczema) patients. Foods and pollens often share conserved proteins that can cause a reaction if a sensitized patient is exposed to either the pollen or the food. Birch pollen is known to cross-react with a variety of foods, such as almonds, apples, carrots, hazelnuts, etc. Sometimes these foods only cause inflammation or symptoms seasonally, when birch pollen is in the air (springtime), but it is also possible for the reactions and symptoms to occur every time the food is eaten.
Once the triggers are discovered, strategies may be put into place to better protect and manage our patients. When the inhalant allergies are known, patients can stay indoors during high pollen or poor air-quality days. Patients can choose moderate exercise and breathe in through their noses to minimize particulate passage into the lungs. In addition, air filters can be used to minimize indoor antigens and pollutants. The elimination of indoor antigens may include the use of HEPA filters, regular high-heat cleaning and drying of bedding, lower indoor humidity (<50%) and mold remediation. In several intriguing studies, green building practices significantly decreased asthma symptoms and exacerbations.
The replacement of essential nutrient cofactors such as magnesium, selenium, zinc, fatty vitamins (A,D,E,K), B-vitamins (mitochondrial support) and essential fatty acids can provide the basis for cellular repair. Additional nutritional (vitamin C, N-acetylcysteine, glutathione, etc.) and herbal supplements can improve antioxidant status and decrease chronic inflammation to restore immunological tolerance.
Gastrointestinal health plays an essential role in programming immune tolerance for the entire body. The provision of probiotics and the restoration of gut health and barrier functions is just as important as respiratory health. Studies indicate that increased consumption of plant-based foods reduces asthma risks; these foods can also improve gut microbiome diversity. We can use food allergy and sensitivity test results to remove reactive, inflammation-causing foods. The results can also guide us in the selection of fruits and vegetables for a healthier diet. In addition to dietary plant intakes, herbal supplements such as curcumin, quercetin and luteolin can also contribute anti-inflammatory effects.
A study of breathing exercises (guided Pranayamas) in stable asthmatic adults demonstrated improvements in symptoms, activity, and quality of life; these subjective improvements were associated in improvements in spirometric volumes, lung capacity, and peak flows. Breathwork, and other mind-body stress management techniques may have a significant effect on immune function, digestion, the gut microbiome and psychological resilience, all of which may improve the quality of life in our asthmatic and atopic patients.
In conclusion, asthmatics and others with respiratory and allergic disorders may be at increased risk of infection during the COVID-19 pandemic. With an understanding of how viral infections exacerbate asthma and lung inflammation, steps can be taken to support our patients and minimize their risks.
In this webinar, Dr. Chris D. Meletis, ND, shares research on COVID-19 as it pertains to airway, allergies, and sensitivities, and how identifying allergens and cross-reactivities can help patients better understand, and potentially minimize, their overall immune burden to support homeostasis during excess allostatic load.
For additional information on CDC-recommended extra precautions for asthmatics, please visit https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html
Anderson JO, Thundiyil JG, Stolbach A. Clearing the air: a review of the effects of particulate matter air pollution on human health. J Med Toxicol. 2012;8(2):166–175.
Agarwal D, Gupta PP, Sood S. Assessment for Efficacy of Additional Breathing Exercises Over Improvement in Health Impairment Due to Asthma Assessed using St. George's Respiratory Questionnaire. Int J Yoga. 2017;10(3):145–151.
Bartuzi Z, Kaczmarski M, Czerwionka-Szaflarska M, Małaczyńska T, Krogulska A. The diagnosis and management of food allergies. Position paper of the Food Allergy Section the Polish Society of Allergology. Postepy Dermatol Alergol. 2017;34(5):391–404.
Berthon BS, Wood LG. Nutrition and respiratory health--feature review. Nutrients. 2015;7(3):1618–1643.
Conticini E, Fediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollution. Published online 4 April 2020. https://doi.org/10.1016/j.envpol.2020.114465
Del Giacco SR, Firinu D, Bjermer L, Carlsen KH. Exercise and asthma: an overview. Eur Clin Respir J. 2015;2:27984.
Dilley MA, Phipatanakul W. Environmental control measures for the management of atopy. Ann Allergy Asthma Immunol. 2017;118(2):154–160.
Hosseini B, Berthon BS, Wark P, Wood LG. Effects of Fruit and Vegetable Consumption on Risk of Asthma, Wheezing and Immune Responses: A Systematic Review and Meta-Analysis. Nutrients. March 2017;9(4):341.
Murray CS, Simpson A, Custovic A. Allergens, Viruses, and Asthma Exacerbations. Proc Am Thorac Soc. 2004;1(2):99-104.
Pascal M, Perez-Gordo M, Caballero T, et al. Microbiome and Allergic Diseases. Front Immunol. 2018;9:1584.
Popescu FD. Cross-reactivity between aeroallergens and food allergens. World J Methodol. 2015;5(2):31–50.
Ryhal B. Viral Disease, Air Pollutants, Nanoparticles, and Asthma. Bronchial Asthma. 2011;267–283.
Santana FP, Pinheiro NM, Mernak MI, et al. Evidences of Herbal Medicine-Derived Natural Products Effects in Inflammatory Lung Diseases. Mediators Inflamm. 2016;2016:2348968.
Schlichte MJ, Vandersall A, Katta R. Diet and eczema: a review of dietary supplements for the treatment of atopic dermatitis. Dermatol Pract Concept. 2016;6(3):23–29.
Sjoberg V. Heal Your Gut with the 4R Program. https://chopra.com/articles/heal-your-gut-with-the-4r-program Accessed 09 April 2020.
Wahbeh H, Haywood A, Kaufman K, Zwickey H. Mind-Body Medicine and Immune System Outcomes: A Systematic Review. Open Complement Med J. 2009;1:25–34.
Wright LS, Phipatanakul W. Environmental remediation in the treatment of allergy and asthma: latest updates. Curr Allergy Asthma Rep. 2014;14(3):419.
Wu D, Lewis ED, Pae M, Meydani SN. Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance. Front Immunol. 2019;9:3160.
www.CDC.gov People Who Are at Higher Risk for Severe Illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html Accessed 09 April 2020.

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...